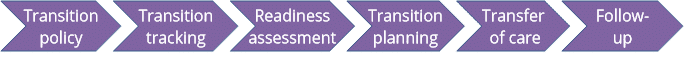
The Six Core Elements are the basic components of the health care transition process. They are designed to be used for pediatric, family medicine, med-peds, and internal medicine practices, but they can also be used in pediatric and adult specialty practices. They were designed by Got Transition™, an initiative of the National Alliance to Advance Adolescent Health. The Got Transition™ website provides a wealth of resources and training on health care transitions. Here is a description of each, with sample documents you might consider for your practice.
© Got Transition™/Center for Health Care Transition Improvement, 01/2014. Got Transition™ is a program of The National Alliance to Advance Adolescent Health supported by U39MC25729 HRSA/MCHB. www.GotTransition.org
Let’s talk about the transition policy. This is a written description of a practice’s approach to transition. It provides information about when and how the transition process starts, gives a general description of the transition process, and describes the role of the provider in the planning process. Developing a practice-specific policy (if your practice doesn’t already have one) can be one of the first steps in improving care delivery for your adolescent patients.
Here's an example you can share with other providers in your practice and with staff. It is also important to share the policy with patients and their families or caregivers so that everyone has the same expectations. https://www.gottransition.org/resourceGet.cfm?id=221
Transition tracking starts with identification. You can use electronic medical records to "flag" patients of transition age (12 years and older) and to help you keep track of their individual transition plans, readiness assessments, goals, and other transition materials. Checklists (like the one developed by the Child Neurology Foundation) can help you keep up with this information.
https://www.childneurologyfoundation.org/wp-content/uploads/2016/04/B_TransitionChecklist.pdf
Transition readiness assessments help providers identify patient needs and help clarify goals for making the transition. Standardized questionnaires ask patients and their parents/caregivers about common adult health care issues. Common questions include those about self-care, managing activities of daily living (for example, feeding, hygiene, taking/managing medications, etc.), keeping and making appointments, talking with health care providers, and monitoring health issues. There are several validated questionnaires, most of which are available in both patient and parent/caregiver versions. Many are available in multiple languages and are designed for patients with lower health literacy. Some are self-assessments, and others are designed to be administered by providers. One has been designed specifically for patients with intellectual and developmental disabilities: the American College of Physicians’ Transition Readiness Assessment for Youth with Intellectual Disabilities or Developmental Disabilities. Other readiness assessments have been (or are being) validated for use in this population. The Resources section of this webpage contains links to other tools, but here is an example of a self-assessment for pediatric patients, the UNC STARx Transition Readiness Questionnaire, to give you an idea of what they often contain.
The StarX questionnaire is available as a Word download from:
https://www.med.unc.edu/transition/transition-tools/trxansition-scale/
When should readiness assessment begin?
The patient should be assessed annually starting at age 14. It often helps to assess both patients and their parents/caregivers (at least initially). This is very useful for patients with intellectual disability and for those patients who will be responsible for managing their care on their own (i.e., patients who plan to move out of the house, who go away to college, or who prefer to be totally independent for any other reason). Differences between the reports of the patient and parent/caregiver can help you identify problems and start conversations about setting goals. Parents should be assessed on their own, if patients have intellectual disability and require very substantial support, if they are medically fragile, if they are nonspeaking/non-verbal, or if they need guardianship.
Developing a patient’s individual transition plan is one of the most important parts of the entire process. Here are the goals of the plan.
- To prepare adolescents to manage their own health care
- To empower adolescents and their parents to function in the health care system
- To identify appropriate health care providers
- To communicate with those providers.
The transition plan itself has these components:
- A complete medical summary - The plan should contain a detailed summary of all of the patient’s medical, surgical, and psychiatric conditions. You can download this three-page sample from:
https://www.gottransition.org/resource/?2022-coding-tip-sheet - The patient's understanding and self-management skills– The plan should include descriptions of both the patient’s understanding of their condition and their self-management skills. Providers should be sure to include information about the patient’s understanding of their prognosis and of the effect that their condition has on their reproductive health. This information is especially critical information for patients with intellectual disabilities who will be managing their care on their own.
- Results of the readiness assessments
- Patient and family preferences for care - It is important to capture and share patient and family preferences for adult services (including preferred hospitals and providers if they have been identified) and goals of care.
- The planned timing of the transition- Scheduling the appointment in consideration of the patient’s birthday as well as benefit plan constraints.
- Activities before the transfer - Labs, imaging, evaluations, referrals, and any other interventions that will be done before transfer.
- Emergency plans, advanced care plans, guardianship (if applicable)– Patients should have emergency contact information in their record, as well as any advance care plans that have been developed. See the section on guardianship for more information, but remember that not all people with I/DD need or should have guardians. Additionally, North Carolina makes it possible for people with mental health needs to write and file advanced directives about how they wish to be treated in the event of a mental health emergency.
Here's a sample transition planning sheet:
https://www.gottransition.org/resourceGet.cfm?id=226
What to cover during the planning visits
A lot of information goes into the transition plan. That means that you, your patients, and their parents/caregivers have a lot to discuss. You should plan to start with your patients' medical condition. What do they understand about their health, their overall prognosis, and how their medical condition(s) will affect their health in the future. Also be sure to discuss their current treatment plan, what they know about it, and how it may change as they age. Always reinforce their knowledge about troubling signs and symptoms, especially those that need urgent/emergent care. And always check in with both patients and parents/caregivers about their mental health. This can be a very stressful time for everyone.
Because their bodies are developing and changing, adolescents have different needs for medical information than they had as children. There are additional suggestions about what to include in the planning visits in the section on working with adolescents.
The planning visit is very important! There is a lot to cover in the initial visit, so you may want to allot extra time. You may need to have a visit that is separate from your patient’s regular follow-up appointments.
If you are wondering about billing and coding for these kinds of appointments, you can find additional information in the American Academy of Pediatrics’ “2018 Coding and Reimbursement Tip Sheet for Transition from Pediatric to Adult Health Care,”
https://www.gottransition.org/six-core-elements/payment.cfm .
Eventually, it will be time to transfer your patient to the new provider. His or her condition should be as stable as possible when it's time.
Compile your transfer documentation before your patient's first visit. The transfer documentation package includes their medical summary, care plan (and emergency plan), final transition readiness assessment, condition fact sheet or resources (for patients with rare conditions), and legal documentation if needed. A transfer letter should also be sent along with the package.
You should notify your patient and their parents / caregivers that you will continue to be their provider (and responsible for their care) until they are seen in the adult provider’s clinic.
The transfer isn't the end of the transition, though. Patients may continue to need monitoring during the transfer, and pediatricians may continue to be involved in their care.
Here's a sample letter for your consideration:
https://www.childneurologyfoundation.org/wp-content/uploads/2017/08/E1_TransferLetterSample.pdf
And here's a sample care plan:
http://www.childneurologyfoundation.org/wp-content/uploads/2017/08/E2_PlanofCare.pdf
What if you can't find an appropriate adult care provider?
In some cases, you won’t be able to readily identify an appropriate adult provider. This often happens when patients have rare neurological, metabolic, or genetic disorders, certain neurodevelopmental conditions, or complex neurobehavioral disorders or if the patient lives in an area with limited access to care. If this happens, you may decide to continue to treat the patient through adulthood, in which case the patient can still make the transition to an adult model of care within a pediatric practice. Providers must continue to help patients search for an adult provider until one can be identified.
The final step in the process is to follow up with patients and families to assure that the transfer to the new practice is working. Congratulations on helping your patient move to an appropriate source of medical care.
