Behavioral Health Crisis
Primary care providers (PCPs) who work with patients who have intellectual/developmental differences (I/DD) may get calls from family member or caregivers* trying to manage a behavioral crisis. Frequently, the person with I/DD has become aggressive, agitated, or uncooperative to the point that the caregiver is concerned about the person's safety or the safety of others. To reduce the danger, the PCP must evaluate the situation to find the best care to provide safety for the patient and for the caregiver.
PCPs may also see patients who are not aggressive or agitated but whose behavior puts them at risk of harm for some other reason. Among the conditions to evaluate and rule in or out are major psychiatric disorders, which affect people with I/DD more frequently than their typically developing peers. Although aggression and agitation can be associated with major psychiatric disorders, when these are not present, symptoms and causes may be more subtle and difficult to tease out.
This page reviews the assessment process and provides resources for immediate and ongoing care of patients with either type of crisis.
Among people with Intellectual/Developmental Differences (I/DD), most behavioral health crises are one of two types. The first, and most common type, are those marked by either extreme aggression or agitation, which can be driven by an array of sources. The second type of crisis are those presenting with symptoms of a co-occurring mental health disorder.
John and Maria provide examples of the two types. Both need an assessment and a plan for care, but there are differences in how they should be handled.
To begin, let's look at John's situation.
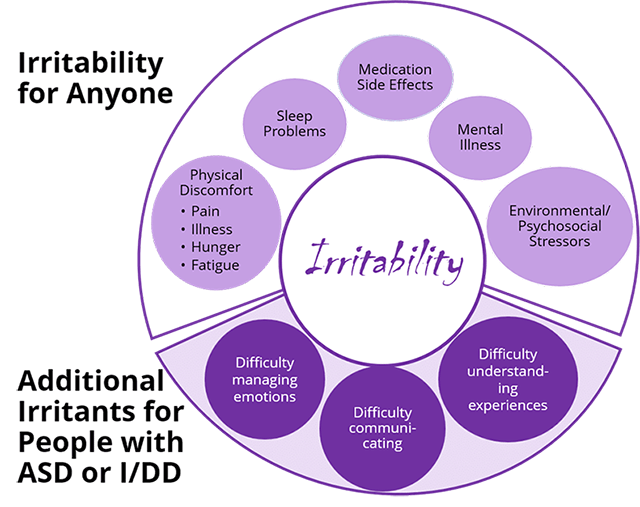
"Irritability"
Most behavioral crises among people with I/DD are characterized by aggression or extreme agitation, as is the case with John. Lecavalier (2006) noted that children with ASD often demonstrate abnormal sensitivity and a tendency to exhibit uncontrolled anger or aggression. Up to 30% of children with ASD have symptoms of “irritability,” including aggression (25%), severe tantrums (30%), and deliberate self-injurious behavior (16%). This is very problematic in young children and particularly dangerous in adolescence, especially among boys. Let's look first at irritability and its causes.
Irritability can escalate in severity to the point of crisis in two ways.
- Severe mood lability and agitation: yelling, flopping, kicking, screaming, prolonged tantrums, bolting away, and low tolerance for frustration.
- Aggressive behaviors directed at self or others:
- Biting, spitting, kicking, hitting, throwing things
- Self-injury such as head banging, wrist biting, slapping, scratching self
- Destroying property
Acute on Chronic
The vast majority of presentations with aggression and agitation are “acute on chronic,” meaning a recent worsening of longstanding challenges involving explosive behavior. Caregivers, and especially families, may have a raised threshold for what constitutes an emergency because of their chronic exposure to very challenging behaviors. Families may be fearful of calling 911 for help and also about potential negative experiences in the emergency room. Most explosive episodes will remit in minutes to hours, and having extra people in the immediate area often maintains safety in the meantime. The need for transportation to the ED is rare, but there are important exceptions.
* Many people with I/DD receive care from family members, while others live in settings with paid caregivers. Here, the term "caregivers" is used to be more inclusive, but it is important to recognize the special strain on family members arising from behavioral crises.
Co-occurring Psychiatric Disorders and I/DD
Psychiatric disorders are more common among children who have I/DD than among the general population—from 30 to 50%, compared to 8 to 18% among typically developing comparison groups (Munir 2016). That said, behavioral problems commonly observed among people with I/DD may or may not indicate a co-occurring psychiatric disorder. Diagnosing mental disorders is challenging, and the goal is to strike a balance between identifying appropriate avenues for intervention while avoiding inappropriate psychiatric diagnostic labels and treatments.
Now, let’s meet Maria.
Overlapping Symptoms
The great difficulty in identifying psychiatric disorders among people with I/DD is that it is often difficult to decide which disorder is responsible for any given symptom. For example, a person whose symptoms include poor self-care or weight loss might also have Depressive Disorder or Anxiety. A person with ASD who has repetitive behavior might also have Obsessive-Compulsive Disorder. In John's case, the aggressive behavior might also belong to a Conduct Disorder. A child diagnosed with Attention Deficit Hyperactivity Disorder might experience a manic episode related to Bipolar Disorder in his teens. Once considered to be rare diagnoses among people with I/DD, primary care providers will increasingly encounter patients with these disorders, particularly among those with mild ASD and most often in teens and adults.
Depression with suicidal thinking and/or behavior is also now understood to be more common among those with mild ASD than among other people (Risha, Fahad, and Mashura, 2014). PCPs should consider screening patients with ASD beginning at age 11 for Depression and Suicidality on well care visits.
Whether the crisis is spurred by aggressive/agitated behavior, like John's, or one, like Maria's, where nonviolent behavior results in the patient's self-harm, the PCP's first steps will be to:
- Evaluate the severity of the episode and the safety of the patient, and when appropriate, of the caregivers
- Identify and rule out potential medical drivers of the behavior, and depending on the symptoms, consider whether there might be a co-occurring psychiatric disorder
- Using this episode as a template, develop a treatment plan and an emergency plan with the patient and caregiver(s).
Understanding the "topography" of the outburst
- How often do these outbursts occur? How long do they last? What happens?
- What does the worst episode look like? What does the most minor episode look like?
- Does the patient cause physical harm to others? How? Who are the targets? Parents, siblings, infants, pets? Is there property destruction? Is the client injuring him- or herself? How does he or she do it? Biting, hitting, head banging?
- What is the extent of those injuries to date?
- Are eyes/orbits being hit, windows/glass broken? Are ears being hit? How hard? Is there bruising?
- Is elopement/running away part of the episode? How often is this a component?
- How far from home has the client gone? Does the client respond to verbal directions to stop? Is there any elopement/running away not associated with an anger episode?
- Are there environmental hazards in the area—pools or bodies of water, busy streets?
Assessing severity and safety
- Remembering that aggressive outbursts are often "acute on chronic," what motivated the caregiver to seek help today, rather than before? What is the worst injury anyone has sustained?
- What is the worst damage the client has caused?
- If the client elopes/runs away, have there been close calls or injuries?
What does the caregiver do?
- How does the caregiver handle this extreme behavior? What is the result? Are there others in the home who help?
- What does the caregiver do to redirect the client and end the outburst?
- Are restraints being employed? How are they done? Who does them? Does using restraints place the patient or caregiver at risk for injury? Has the caregiver struck or otherwise physically injured the patient?
What steps have been taken to improve safety of the environment?
- Does the home have door alarms and adequate door locks?
- Does the caregiver keep sharp objects and projectiles from key areas? If there is a yard, is it fenced?
- Are there other steps the caregiver has taken?
How is the caregiver's health and well-being?
- Does the caregiver have symptoms of Depression and/or Anxiety?
- Is he or she receiving treatment?
- What supports does he or she have for managing the client's behaviors?
- Does he or she have access to respite?
- Does the caregiver show signs of suicidality?
- Passive suicidal ideation is common among highly stressed caregivers.
- Active suicidality is rare, but PCPs should ask about it.
- Does the caregiver use substances? Which one(s)? How frequently? How much?
- There is emerging evidence that caregivers are at increased risk for Substance Use Disorder, especially in the context of a patient's extreme externalizing behaviors.
Crises associated with explosive behavior and agitation are complex to sort out. They often result from more than one source and may be difficult to assess completely in a primary care setting. Remembering that the patient may have difficulty communicating what the problem is, the place to start is with the most common medical drivers of irritability.
- constipation/encopresis (the effect of which is often underestimated)
- pain
- gastrointestinal
- dental
- secondary to infections (e.g., urinary tract or respiratory)
- premenstrual
- medication side effects
- psychostimulants (common culprit)
- Selective Serotonin Reuptake Inhibitors (common culprit)
A review of the information you gathered to begin the assessment may highlight potential situational or environmental causes of the difficult behavior: Does the patient have difficulty with transitions? Do the episodes occur around mealtimes or bed time?
 The patient’s self-injury is getting progressively worse. Watch for:
The patient’s self-injury is getting progressively worse. Watch for:
- Mental status changes secondary to severe head banging
- Ocular (eye) injury, auricular (ear) injury, dental injury
The patient is at imminent risk for accidental injury or death
- Elopement
- Drowning
Others may be injured by the patient. Examples include:
- An infant in highchair has been knocked over during explosive outburst
- An older teenage patient who has grown quite strong hits his parent or caregiver.
There are other significant risks:
- The patient or the parent/caregiver risks death by suicide
- The caregiver may harm the patient
- The caregiver is impaired and unable to provide care
Work with the patient and caregiver to address the possible medical sources of irritability. Consider the appropriateness of removal or initiation of pharmacologic treatment, with close follow-up based on your comfort level and experience with these medications and/or with input from a psychiatric colleague.
Irritability should not be treated directly with psychiatric medication until you have completed a systematic evaluation of the potential medical and environmental drivers of the aggressive/agitated behavior, unless acute or subacute safety risks are such that the potential benefits of the medication outweigh the potential negative effects. In lieu of a complete review of the evidence for prescribing psychiatric medications for people with I/DD, here are some brief points to consider:
- The research on and drug trials of the use of psychiatric medications with people with I/DD are not extensive, and they have mostly been conducted with people who have ASD, rather than on I/DD with different etiologies.
- Only two medications have FDA approval for treating symptoms of severe irritability in ASD, risperidone for children ages 5–16 and aripiprazole for those ages 6–17.
- Psychiatric medications often have side effects that contribute to irritability.
Whether or not medications seem indicated, ongoing assessment and consideration of medical and situational drivers of irritability will be part of the follow-up. It will also be important to connect patients and caregivers effectively with specialists who can address more complex medical or mental health disorders and with community sources of services and supports. Additionally, if there is no emergency plan in place, or if it needs to be updated, that will be part of the continuing work with patients and caregivers.
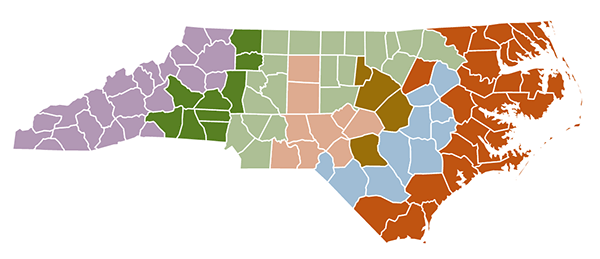
NOTE: If you are a health care provider in North Carolina and wish to consult with a physician at UNC Chapel Hill about your patient’s care, you can call the Carolina Consultation Center’s toll free number at 1-800-862-6264. If you practice in Person, Granville, Vance, Warren, Franklin, and Halifax counties, you can call the NC-Pediatric Access Line (NC-PAL) 919-681-2909 for assistance https://ncpal.org/.
If You Suspect Abuse or Neglect
Unfortunately, people with I/DD have higher rates than the general population of being abused and/or neglected by caregivers or services providers in the home or other care setting. North Carolina law requires that anyone who suspects abuse, neglect, or exploitation of a child or disabled adult (age 18+) report it to the county department of social services in which the person with I/DD lives. A list of NC County Departments of Social Services can be found at https://www.ncdhhs.gov/divisions/social-services/local-dss-directory. Ask for the Child or Adult Protective Services social worker.
Obtaining Emergency Care on Site
Does the family work with some type of behavioral health agency? Do they know the emergency plan with that agency? Do they know how to contact mobile crisis services for their area? Crisis services can be accessed via the LME/MCO for county in which they live. See the link https://www.ncdhhs.gov/providers/lme-mco-directory for the contact information for them.
At home, caregivers who believe that the person with I/DD needs immediate treatment may call 911. When calling 911, it is important for the caller to explain that the person has I/DD, and to request that a Crisis Intervention Trained (CIT) officer respond.
Using the Emergency Department
Sometimes the best course of action is to send the patient to a hospital's Emergency Department (ED). Use the ED sparingly, but it is the right immediate referral when the patient's safety is clearly compromised. It is best to discuss your concerns with the patient and caregiver and have their situation evaluated voluntarily in a facility where involuntary commitment is also possible, if needed. In severe situations like Maria’s, a psychiatric referral to the ED is the best choice.
Particularly when working with patients age 18 and older, be sure to check who the patient's legal guardian is. Adults with I/DD may be their own guardians, or others may fill that role. In the context of an adult who is his/her own legal guardian, a physician, eligible psychologist, or other specifically credentialed behavioral health professional in NC can initiate involuntary commitment if needed. See https://www.ncdhhs.gov/assistance/mental-health-substance-abuse/involuntary-commitments for more detail about that process. You can also call your local magistrate for guidance if needed (open 24 hours a day). The magistrate for your county can be found by going to https://www.nccourts.gov/locations and selecting your county. Alternatively, if responsibility for guardianship of the adult with I/DD is with the county department of social services, then they should be notified https://www.ncdhhs.gov/divisions/social-services/local-dss-directory.
In the extremely rare case where a legal guardian refuses to have the patient evaluated in the ED, after you have determined need, call 911 if harm is imminent, as well as child or adult protective services in the county department of social services. Here is an online directory for all the counties: https://www.ncdhhs.gov/divisions/social-services/local-dss-directory.
Ideally, patients and caregivers should be guided to the closest ED, but remember that some EDs have more experience and comfort than others serving people with I/DD. Do you know which one(s) in your area would be best?
Patients and caregivers should understand that the ED is a good place to rule out medical factors for the crisis, maintain safety, and determine need for admission. That said, caregivers should also understand that most ED visits for explosive behavior will not result in psychiatric or other admission.
In the rare cases when admission is necessary, patients and caregivers should understand that in the current resource climate, there will likely be significant time spent in the ED (sometimes days) before admission, and in some situations, the psychiatric unit with an available bed may be some distance from the patient’s home.
Accessing Crisis and Residential Services through the LME/MCOs
Many patients with I/DD use Medicaid for medical insurance. For their behavioral health care needs and emergencies, the Local Management Entity/Managed Care Organization is the point of contact for services. See the map below, and https://www.ncdhhs.gov/providers/lme-mco-directory for the contact information for them.
Local Management Entities/Managed Care Organizations Map (LME/MCOs)
Longer-term Care
North Carolina operates three developmental centers serving the west, Piedmont, and east: The J. Iverson Riddle Center in Morganton, The Murdoch Center in Butner, and The Caswell Developmental Center in Kinston. All of these facilities provide care for adults (18+) with I/DD and complex medical and/or psychological conditions that cannot be adequately treated in the community. Admission to these facilities can be a long process, and available community options for care must have been tested. The LME/MCO is the starting point. For more information visit https://www.ncdhhs.gov/divisions/dsohf/facilities . Scroll down the page to see links to all three centers and a description of eligibility criteria.
Crisis Services
Referrals for children should be made to the LME/MCO. For adults (age 18+) direct referrals may be made to NC START (North Carolina Systemic, Therapeutic, Assessment, Resources, and Treatment), which provides statewide community crisis support programs for people with I/DD and complex behavioral or mental health needs. Crisis prevention and intervention services are provided through crisis response, clinical consultation, training, and respite. There are three centers in the state that serve the west (out of Statesville, Concord, and Asheville), Piedmont (Durham and Franklinton), and east (New Bern, Wilmington, Greenville). Consult their website for more information, https://www.centerforstartservices.org/locations/north-carolina. NC START is also available for children beginning at age 6 and referrals must go through the LME-MCO.
- The majority of crises among patients with I/DD relate to aggression, explosivity, and anxiety. They are very often "acute on chronic" episodes.
- Assess the medical and physical drivers of irritability, and treat those when possible. Don’t forget that psychiatric medications could be part of the problem.
- Work with the patient and caregiver(s) to plan for future crises. Connect them to appropriate resources—the LME/MCO, which is the gateway to many other services including mobile crisis response teams, and to NC START.
- Pay attention to the health and stress level of family caregivers, and refer them to respite.
- Use the ED sparingly but when the patient's safety is clearly compromised.
- Consider starting treatment with psychiatric medication based on your comfort level with prescribing it, if it seems appropriate, or seek consultation.
- Because people with I/DD are at greater risk than the general population, watch for crises without explosive behavior that may be symptoms of such psychiatric conditions as Depression, Psychotic Spectrum Disorder, Bipolar Disorder, Anxiety, and Suicidality.
Resources
ARCH National Respite Network. (2018). 9 steps to respite care for family caregivers of children and adults with intellectual and developmental disabilities. https://disabilitynavigator.org/article/68325/9-steps-respite-family-caregivers-children-and-adults-intellectual-and-developmental
Carolina Consultation Center. 1-800-862-6264 (toll free). [For practitioners anywhere in North Carolina.]
Crisis Solutions North Carolina. http://crisissolutionsnc.org/ [Mobile crisis units and crisis centers.]
Deb, S., Clarke, D., & Unwin, D. (2006). Using medication to manage behaviour problems among adults with a learning disability: Quick reference guide. https://www.birmingham.ac.uk/documents/college-les/psych/ld/ldquickreferenceguide.pdf
Summary of NC's Current Law on Involuntary Commitment. https://www.ncdhhs.gov/divisions/mental-health-developmental-disabilities-and-substance-abuse/involuntary-commitments
NC County Departments of Social Services. https://www.ncdhhs.gov/divisions/social-services/local-dss-directory
NC Developmental Centers. https://www.ncdhhs.gov/divisions/dsohf/facilities.
NC Local Management Entities/Managed Care Organizations (LME/MCOs). https://www.ncdhhs.gov/landing-page/clone-lmemco-directory, or download the reference sheet.
NC Pediatric Access Line (NC-PAL). (919)681-2909 [For practitioners in Person, Granville, Vance, Warren, Franklin, and Halifax counties. For details, see https://ipmh.duke.edu/content/ncpal.]
NC Systemic, Therapeutic, Assessment, Resources, and Treatment (NC-START). https://www.centerforstartservices.org/locations/north-Carolina [Services for adults.]
Vanderbilt Kennedy Center (Nashville, TN). Health care for adults with intellectual and developmental disabilities: Toolkit for primary care providers. https://iddtoolkit.vkcsites.org/. [This toolkit provides a number of assessment tools for managing behavioral crises.]
References
Ageranioti-Bélanger, S., Brunet, S., D'Anjou, G., Tellier, G., Boivin, J., & Gauthier, M. (2012). Behaviour disorders in children with an intellectual disability. Paediatrics & Child Health, 17(2), 84–88.
Lecavalier, L. (2006). Behavioral and emotional problems in young people with pervasive developmental disorders: Relative prevalence, effects of subject characteristics, and empirical classification. Journal of Autism and Developmental Disorders, 36(8), 1101-1114.
Richa, S., Fahed, M., Khoury, E., & Mishara, B. (2014). Suicide in autism spectrum disorders. Archives of Suicide Research, 18(4), 327–339.
Dr. Rob Christian

We thank Dr. Rob Christian at the Carolina Institute for Developmental Disabilities for the development of this material.
Rob Christian, MD, joined Carolina Institute for Developmental Disabilities in 2009 and is an assistant professor of psychiatry and pediatrics in the UNC School of Medicine. Dr. Christian graduated from the UNC School of Medicine and did his postgraduate training at The Brown University Triple Board Program, which is a combined training program in General Pediatrics, Adult Psychiatry, and Child/Adolescent Psychiatry.
